Abdominal Hernias
A hernia is a protrusion of tissue from one part of your body, through the tissue wall that contains it, into another part of the body. There are many types of hernias and they are named depending on where they occur in your body.
The commonest hernias that effect patients are abdominal hernias. These are hernias that appear in areas such as the groin, umbilicus (“belly button”), the midline of the abdomen or old scars (incisional hernias).
The following information explains more about what specific types of hernia there are, the factors that contribute to a hernia, what problems can occur with hernias if they are not fixed, when should hernia repair be considered, what the surgical options are for repairing a hernia and factors you can control to help any hernia surgery be successful.
Abdominal Hernia Types
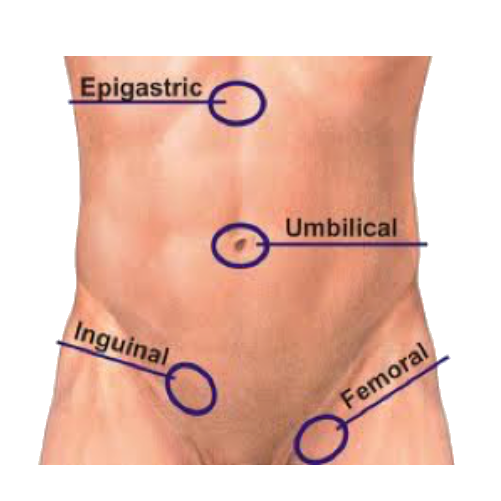
These hernias are generally named depending on their location within your abdominal wall. They are all very common. Up to 10% of the population will develop at least one hernia of this type in their lifetime. If you have had one of these hernias previously, you have a 20% chance of having another type of hernia at the same time or later in life.
The diagram opposite shows where these common hernias occur. There are certainly large differences between how often they occur in men and women for some of these hernias.
This is the most common type of hernia making up approximately 70% of the total number of abdominal hernias seen. Most patients with this problem are male with 9 out of 10 patients being men. The hernia occurs through a region in the groin called the “inguinal canal”. The inguinal canal is there to allow certain anatomical structures to pass into and out of the abdomen. In men, the canal contains the spermatic cord (which contains the testicular blood vessels, nerves and the vas deferens from the testicle) and in women it contains a ligament from the uterus called the round ligament with the same nerves found in men.
Most patients notice a lump in the groin, just above the groin crease. This may be associated with pain or a vague, dragging discomfort that can be felt in the testicle in men. In very large inguinal hernias in men, the swelling may reach down into the scrotum and in this case, it is called an “inguinoscrotal hernia”.
This is the second commonest hernia making up around 20% of hernias. They can occur from within the belly button itself (umbilical hernia) or just next to it (paraumbilical hernia). They are a little more common in women but only just. Again, a lump is what is usually noticed, or a change in the shape of the belly button from an “inny” to an “outy”. These hernias can be associated with pain as well but it is less common than pain with inguinal or epigastric hernias.
An epigastric hernia occurs in the midline of your abdominal wall anywhere from just above your belly button up to your breast bone (sternum). These can often be very small but painful hernias. Often, you do not realise there is a lump there until your GP finds it when she or he is looking for a reason for your pain. They make up around 5% of abdominal wall hernias.
Femoral hernias are a variation of a groin hernia but are different to inguinal hernias because they occur through an opening in the muscles and ligaments of the groin below the inguinal canal. The area these hernias occur through is not surprisingly called the “femoral canal”.
They are much less common than inguinal hernias, making up less than 5% of all abdominal hernias. Whereas inguinal hernias are more common in men, femoral hernias are much more common in women. Again, the main symptom is a lump but it is normally found below the groin crease and sitting in an area at the very top of the inner thigh.
Hernias that occur in old wound scars from previous operations (eg bowel surgery, laparoscopy, cholecystectomy etc…) are called incisional hernias. They occur in previous incisions through weakened scar tissue. They can range from being very small to very large lumps that can contain bowel and other organs.
There are many reasons and factors that lead to the development of a hernia. It is unusual that one single issue is the sole cause. Hernias generally occur at points of weakness in a muscle and tendon wall. Areas such as your belly button or groin are weak points in our anatomy and in some people, these areas give way to form a hernia. This doesn’t occur in every person however and there are other factors at play.
Our research has shown that the following issues can be a contributor to hernia formation:
• Obesity
• Repetitive or very strenuous physical activity
• Chronic cough and smoking
• Previous surgery to the area (including previous hernia repair)
• Previous wound infection (incisional hernia)
• Diabetes (incisional hernia)
• A previous hernia elsewhere in your body
• Collagen and connective tissue disorders
Many people in the community will go through their entire life with a hernia and it will give them no symptoms or trouble at all. Some people do not even know they have a hernia. The risk of leaving a hernia unrepaired is generally low in the short term provided there has been very little pain or other concern. As time goes on however, there is a risk a hernia may become bigger and complications can develop.
If a patient has symptoms besides a lump, the most common thing that they complain of, is discomfort or pain that is usually related to when the hernia bulges out. As long as the hernia can go back in, this is a low risk. Sometimes however, a hernia can become stuck (irreducible) and this can result in severe pain. If bowel is stuck in that hernia, it then becomes urgent that the hernia contents are returned into the belly promptly and usually within hours. If this does not happen, there is a risk that whatever is stuck in the hernia could lose its’ blood supply permanently (strangulated), become gangrenous and need to be removed.
The lifetime risk of developing strangulation for all hernia types is about 4% a year. For femoral hernias, this risk is much higher however – estimated to be as high as 25%. Unfortunately, we do not have any guaranteed way of determining which hernias will develop problems later in life and which will not.
There has been much debate regarding when, or even if, all hernias should be repaired.
Sometimes your GP will diagnose a hernia due to the fact you have noticed a lump where the hernia is. In this situation, provided you are well enough to undergo an operation, any hernia you can visibly see or feel, should be considered for a repair. This is especially the case if you are getting other symptoms such as pain in the hernia. This will involve a review by a surgeon experienced in the various types of hernia repair available for that particular problem.
The other circumstance which commonly occurs is a hernia is diagnosed after a scan of some type (usually and ultrasound or CT scan) is done to consider a problem such as groin pain, but there is no obvious lump present. In this situation, even though your scan says you have a hernia, it may not be the cause of your symptoms. It may in fact make your problem worse if surgery is performed in some of these situations.
When it is not clear that a hernia can be seen or felt by you or your GP, the decision to operate should only be made after you have had a thorough history taken and physical examination done by a specialist surgeon experienced in the treatment of not just hernia disease, but also musculoskeletal or abdominal pain from other causes.
Ultimately, if there is a concern that you have a hernia, consultation with a hernia surgeon is essential not just to decide if the hernia needs repair, but also to assess you for fitness for surgery. In some circumstances, if you have other major medical problems such as heart or lung disease, it may be deemed safer to not operate on a hernia.
There are many different techniques for repairing hernias. The best operation for you will depend on many things including:
• what type of hernia you have
• whether this is the first time this hernia has been repaired
• the size of the hernia defect (how wide the hole in the muscle is)
• is there more than one hernia
• your general health
For some very small hernias (eg epigastric and some umbilical hernias), just suturing (stitching) the hernia is enough. More commonly however, most hernia repairs with bigger defects, involve strengthening the repair with mesh of some type. There are many types of mesh available depending on the job that is required of the mesh but all of them cause the body to lay down scar tissue in the mesh across the defect without having to pull the weak tissue together under tension. This acts as patch across the opening and has led to excellent results since it was introduced back in the 1980’s.
Besides whether mesh is used, the other big decision when repairing a hernia is to decide whether the operation is performed with a direct incision over the hernia (open repair) or using a keyhole approach (laparoscopic repair).
Every type of technique used has its’ own set of advantages and disadvantages and different set of risks. Which type of operation that is best for you will depend upon your assessment by your surgeon and what he or she is skilled in performing.
It is best to consult with a surgeon that is skilled in all aspects of hernia surgery and someone who performs a large volume of these operations regularly. It is an ever-changing area of surgery with new techniques, materials and research findings emerging every year. These changes make it essential to keep up with this very dynamic area to provide the best practice for patients.
There are a few important things you have control of and can do prior to surgery that can have an enormous improvement to your surgery success rate:
- Smoking cessation is one of the most important things that can make a difference to your hernia repair. If you are smoking at the time of your operation, besides the general risks associated with this, your chance of your hernia coming back after surgery is at least 4 times more likely than in people who are not smoking. If you need assistance with this, your GP is usually an excellent person to help with this. Alternatively, you can contact the NSW Quitline on 13 7848 or visit the following website: http://www.health.nsw.gov.au/tobacco/Pages/services-to-help-you-quit.aspx
- Weight loss prior to surgery (if you are overweight) is the other major factor that will improve the results of hernia surgery. This is especially the case for umbilical and incisional hernias. Even losing as little as 5kg to 10kg in weight prior to an operation can make a massive difference to the outcome. In some situations, achieving a target weight may be advised prior to an operation going ahead.
- Good skin care around the skin folds where your hernia is situated is required. Any evidence of an active rash or infection at the site of your surgery will result in your operation being delayed until this problem can be treated. If you have any doubts, consulting with your GP or surgeon is essential prior to going ahead with surgery.
- Good blood sugar control for diabetic patients is essential. This will improve you healing after surgery and minimise the risk of infection.
As with most operations, you will need to rest for a period of time after your procedure. In most circumstances after a hernia operation, most people can return to a job with light duties within 2 weeks after the surgery. For jobs that involve heavy lifting or a lot of physical strain however, a six week period where lifting any more than 10kg is not permitted. If you resume heavy physical activity too early after you operation, the chance of the hernia returning is much higher.
I normally recommend you do not drive for a week as well. If you still have significant discomfort after that time, you should not drive until the discomfort settles.
